
Most newborns ( neonates ) show symptoms of jaundice ( jaundice ) three to four days after birth. This jaundice occurs in 40-60% of term neonates and 80% of preterm neonates. This jaundice is normal due to a change in the type of hemoglobin in the red blood cells of the fetus while in the womb to the red blood cells of the baby after delivery. However, there are a number of warning signs that your baby's jaundice could be a disorder.
What are the Signs of an Abnormal Baby Jaundice?
- Has appeared less than the first 24 hours.
- Jaundice persists for more than 8 days in term infants and more than 14 days in preterm infants.
- In three days the baby became increasingly yellowish.
- Followed by a fever.
- The baby looks weak, sleeps constantly, and doesn't want to breastfeed.
- Pampers appear dark yellow-brown urine like tea and pale cream-yellow stools like putty.
- Accompanied by pale stools like putty.
- Yellowish followed by an enlarged belly.
The cause of abnormal jaundice in your baby can be caused by an abnormal flow of bile from the liver to the intestine ( cholestasis ) for various reasons.
Various diseases cause cholestasis in infants aged less than 2 months.
- Biliary atresia.
- Choledochal cyst.
- Alagille's syndrome (paucity of the interlobular bile ducts or arteriohepatic dysplasia).
- Inspissated bile / mucous plug.
- Cystic fibrosis.
- Neonatal Sclerosing Cholangitis.
- Congenital hepatic fibrosis / Caroli's disease.
- Tumor/mass (intrinsic/extrinsic).
- Gallstones.
- Viral infections (Cytomegalovirus, HIV, Herpes, Rubella, parvovirus, Echovirus, adenovirus), Bacteria (Urinary tract infections, Sepsis, Syphilis), protozoan parasites (Toxoplasma), and liver flukes.
There is a history of illness that has the potential to cause abnormal jaundice in your baby.
- Similar symptoms in parents and siblings α1-antitrypsin deficiency, progressive familial intrahepatic cholestasis (PFIC), Alagile syndrome, and cystic fibrosis.
- TORCH infection (Toxoplasma Rubella Cytomegalovirus and Herpes) and Hepatitis in a pregnant mother.
- Fetomaternal ultrasound found a choledochal cyst.
- History of ABO disease or Rh or Rh negative – hemolysis.
- Neonatal infections include urinary tract infections, sepsis, and, viral infections.
- Gastrointestinal symptoms – vomiting, pasty/pale colored stools (assessed by stool color card).
- Dark urine – bilirubinemia.
Biliary atresia.
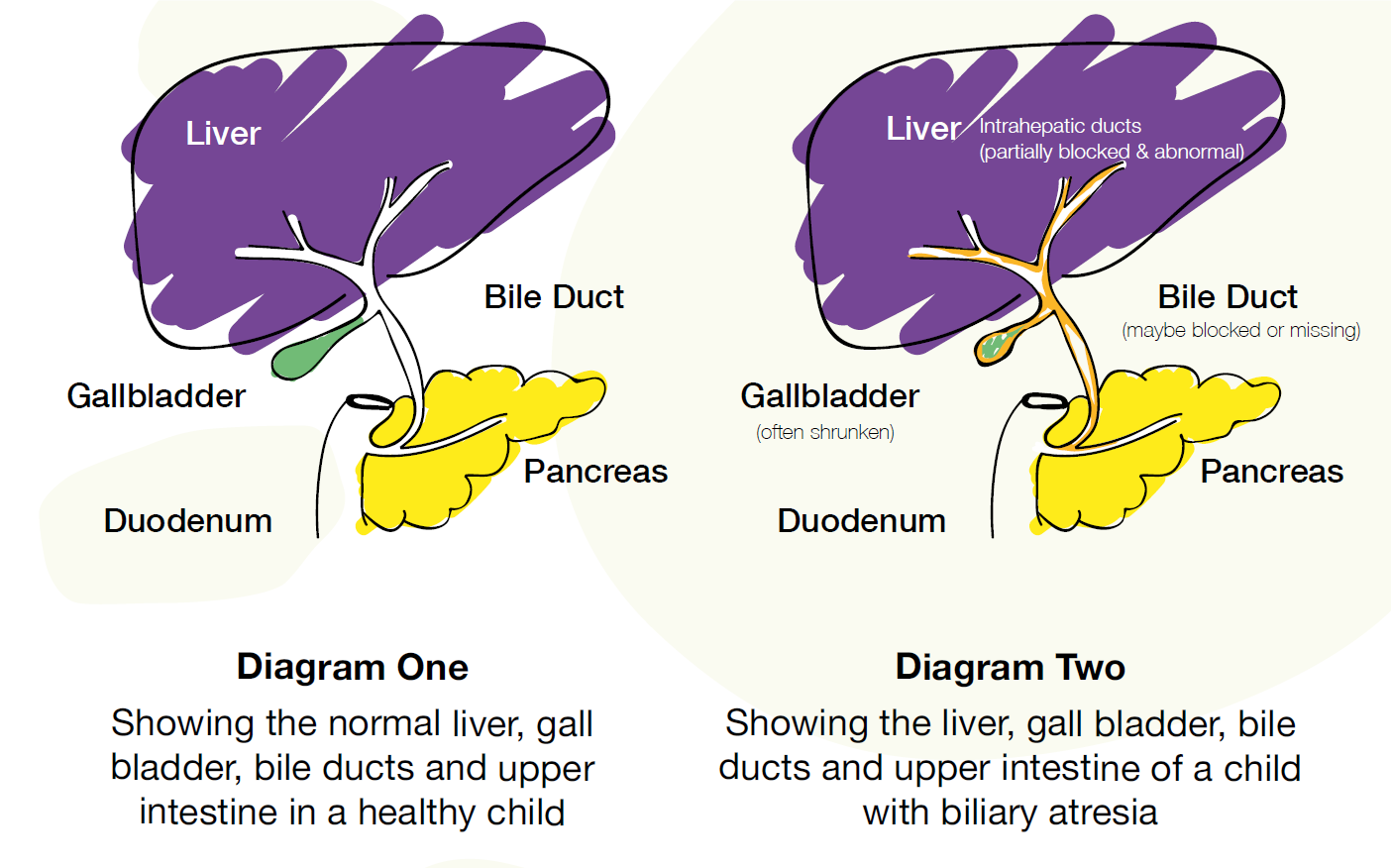
Bile is useful for fat digestion and will color the stool. Biliary atresia literally means a break in the bile duct. This disorder is most common in East Asia, including Southeast Asia. Biliary atresia is a disorder of the bile duct in the form of fibro-proliferative damage so that the flow of bile from the liver to the intestine cannot run since the baby is born. This buildup of bilirubin in the bile will poison and damage the liver, and brain and can end in death.
Why Should Biliary Atresia Be Known at the Early Stage?
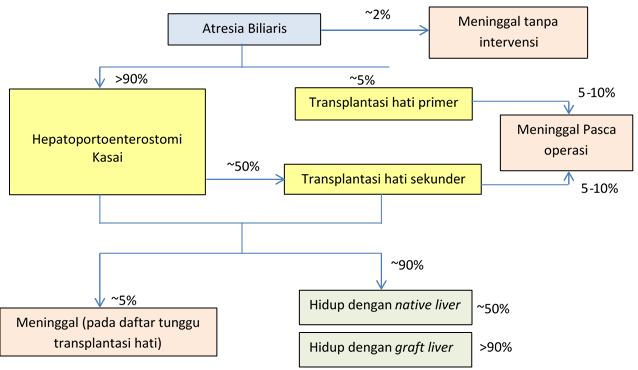
Jaundice due to biliary atresia should be diagnosed as early as possible and taken action immediately (before the age of 3 months) because the baby can be helped by an operation to create an artificial shortcut for bile flow called the Kasai Hepatoportoenterostomy operation. If this surgical assistance is carried out before the baby is two months old, the success of the operation reaches more than 80% so it is hoped that the patient will not die in the first or second year of life and 23% of patients can reach the age of 20 years. If the new Kasai operation is carried out past the age of 3 months, the success rate will decrease considerably, the highest is only around 20%. Delay in treatment will lead to more rapid liver damage and can only be helped by liver transplant surgery, whereas in Indonesia until now there are not many central hospitals that are capable of performing liver transplants except at RSCM Jakarta.
So it is very important for parents to immediately check their babies who suffer from abnormal jaundice with the family doctor and pediatrician. The easiest thing to do is with a stool color card.
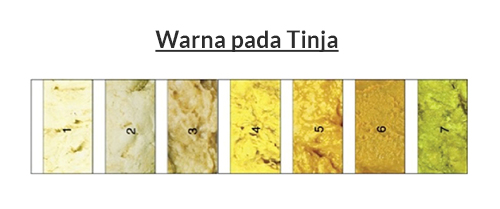
Stool color card
- Delay when first seeking treatment at the health center, is a major problem in Indonesia.
- Data from the pediatric liver disease section at the RSCM national referral hospital show that the average age of patients with abnormal jaundice when they first come is at the age of 4 months.
- The high rate of delay causes a high rate of liver failure and death in patients with biliary atresia.
- Methods for early detection of biliary atresias, such as examination of the color of the stool/feces and the use of a Stool Color Card (KWT)
- The color of the stool in biliary atresia which is very typical is pale (colors 1, 2, and 3)
When should you refer to the doctor?
- Jaundice with onset from birth and not improving by 2 weeks postpartum
- Dark urine color
- The color of the feces is putty/ acolis
- There are signs of liver failure in the form of an increasingly enlarged stomach, red bloody bowel movements ( hematochezia ), vomiting blood ( hematemesis ), black bloody bowel movements ( melena ), difficulty gaining weight, weak children looking very jaundiced and having seizures
The article was written by dr. Leo Rendy, Sp.B (K) Ped (Pediatric Surgeon at EMC Sentul Hospital).
