
Percutaneous Coronary Intervention (PCI)
Not much is known that coronary heart disease or blockage of the coronary arteries can be overcome through the Percutaneous Coronary Intervention (PCI) procedure or sometimes also known as percutaneous coronary intervention. What is the procedure like and what needs to be considered during, before and after undergoing this procedure? Read more in the article below.
What is Cardiac PCI?
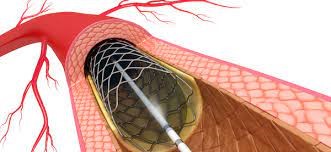
PCI is a non-surgical interventional procedure to dilate or open narrowed coronary arteries using balloons or stents . The process of narrowing of the coronary arteries can be caused by atherosclerosis or thrombosis.
What causes someone to do PCI action?
Atherosclerosis causes narrowing of the heart arteries. Complaints can be like left chest pain that comes and goes or doesn't even cause clinical symptoms, so patients with Coronary Heart Disease (CHD) generally have no significant complaints.
Heart Attack Risk Factors:
- Smoke
- Hypertension
- Obesity
- Lack of Activity
- Family History
- Diabetes mellitus
- Cholesterol
- Stress and anxiety
With the factors mentioned above, it will accelerate the buildup of plaque in the coronary arteries.
Patients with CHD who have taken routine medication and changed their healthy lifestyle but still have complaints of recurrent chest pain, patients with heart attacks, patients with positive treadmill test results should undergo coronary angiography to assess whether there is narrowing of the heart arteries, if narrowing is found in significant cardiac vessels should be performed PCI procedure.
What is the PCI procedure?
Such as catheterization, the PTCA procedure uses sterile clothing from the hospital, an infusion line is placed on the left hand, the patient's position is supine on the action table, then electrodes are placed on the chest to monitor the condition of the heart during the procedure, the nurse will perform an aseptic procedure / clean the action access site, the doctor will provide local anesthesia to blood vessels that have been aseptically treated. Then the catheter (sheath) is inserted up to the coronary arteries of the heart, contrast fluid will be inserted to assess the stenosis / narrowing. To enter the narrowed coronary arteries, guided by a guide wire .
After the guide wire passes through the constricted area, the balloon is inflated (inflation) in the narrowed area. After the blood vessels are opened, usually a stent is placed with the aim of keeping the blood vessels open.
There are 2 types of stents on the market, namely bare metal stents and drug eluting stents . The stent that has been installed will stick to the coronary arteries.
What are the preparations before undergoing a PCI procedure?
Preparation Before PTCA or PCI Action:
- Perform blood laboratory tests
- Perform cardiac recording/electrocardiography (EKG)
- Photo of the chest (X-ray)
- Fasting for 4-6 hours before the procedure is carried out, to take medicine as usual
- Get an explanation of the action procedure
- Sign the informed consent form
Post PTCA or PCI Patient Care:
- The patient is allowed to eat/drink as usual
- If the procedure is performed on the lower extremity, the area of action should not be bent for 12 hours
- If the action is performed on the upper extremity, the action area should not be bent or grasped after the action.
- If there are no complications or other abnormalities, the next day you can be allowed to go home.
- Usually this action only takes a few days of treatment, if there are complications.
What are the risks and side effects of this procedure?
Risks such as bruising on the wrist or groin due to catheter insertion, allergic reactions to contrast, and impaired kidney function due to excessive contrast agent. More serious complications such as stroke, fatal rhythm disturbances such as Ventricular Tachycardia (VT)/Ventricular Fibrillation (VF), Myocardial Infarction, Aortic Dissection, and death on PCI or PTCA procedures. Complications are more common in patients with severe disease, aged > 75 years, co-existing diseases such as kidney and diabetes, decreased heart pump, and many and severe narrowings.
Article written by dr. Ike Adriana, Sp.JP, FIHA (Heart and Blood Vessel Specialist at EMC Pulomas Hospital).
